Introduction
Vasectomy, a widely practiced surgical method for male sterilization, is typically regarded as safe and effective. However, its long-term physiological impact on testicular health remains a subject of evolving research. One critical yet underexplored area is testicular vascular dysregulation — the disturbance of normal blood flow dynamics within the testes following vasectomy. This dysregulation can have downstream effects on spermatogenesis, hormonal signaling, and testicular function, potentially contributing to chronic pain syndromes and fertility challenges in rare reversal cases.
This article explores the pathophysiological mechanisms linking vasectomy with altered testicular hemodynamics, integrates emerging imaging and histological data, and highlights implications for clinical practice and post-operative monitoring.
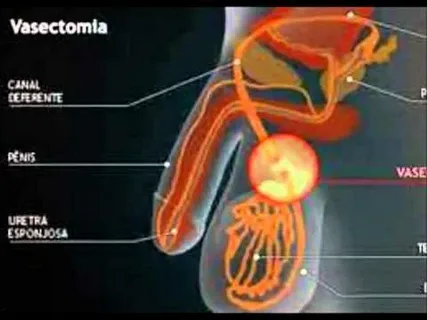
Understanding Testicular Vascular Anatomy
To appreciate the effects of vasectomy on vascular regulation, it’s vital to understand the complex architecture of testicular blood supply. The testicular artery, arising from the abdominal aorta, provides oxygenated blood to the testis, while venous outflow is managed by the pampiniform plexus, a network that also plays a role in thermoregulation.
Vascular homeostasis within the testes is finely tuned. Even slight alterations in blood flow or venous drainage can result in tissue hypoxia, impaired spermatogenesis, or varicocele development. Because vasectomy involves ligation or cauterization of the vas deferens — which travels in close proximity to testicular vessels — unintended vascular consequences are plausible, especially when post-operative fibrosis or inflammatory responses occur.
Mechanisms of Vascular Dysregulation Post-Vasectomy
1. Inflammatory Sequelae
After vasectomy, the body often mounts an immune response to the sudden obstruction of sperm transport. Spermatozoa that can no longer exit the testis accumulate and may rupture, spilling antigenic material into surrounding tissues. This triggers localized granulomatous inflammation, which can compress small vessels and alter microvascular perfusion.
Proinflammatory cytokines such as TNF-α, IL-1β, and IL-6 released in response to sperm leakage can lead to endothelial dysfunction. This affects the nitric oxide (NO) signaling cascade essential for vasodilation, thus predisposing to vasoconstriction and ischemia in localized testicular regions.
2. Fibrotic Remodeling
Over time, the vasectomy site undergoes fibrotic changes. When these fibrotic bands extend to nearby vascular structures, particularly the pampiniform plexus or perivascular regions, they can obstruct venous return. This phenomenon mimics the pathophysiology of varicocele — known to impair testicular thermoregulation and function.
Experimental models have shown that fibrosis in the spermatic cord post-vasectomy can distort the alignment of the testicular artery and its branches, leading to increased vascular resistance and reduced blood flow velocity on Doppler ultrasound.
3. Venous Congestion and Retrograde Pressure
Vasectomy-induced obstruction may not be limited to the vas deferens but could affect surrounding structures, including veins. This can result in retrograde venous hypertension, a condition where elevated venous pressure hampers effective arterial inflow. Over time, this leads to stagnation of blood, accumulation of metabolic waste, and oxidative stress within the testis.
Increased hydrostatic pressure also promotes vascular permeability, resulting in interstitial edema and further distortion of the microvascular environment.
Clinical Manifestations of Testicular Vascular Dysregulation
1. Post-Vasectomy Pain Syndrome (PVPS)
One of the most debated long-term complications of vasectomy is PVPS — chronic scrotal pain lasting more than three months after the procedure. Although multifactorial, testicular vascular dysregulation likely contributes to this syndrome. Altered perfusion may sensitize peripheral nerves or induce ischemic changes that promote nociceptive signaling.
Doppler imaging in some PVPS patients has revealed increased resistive indices, supporting the hypothesis of impaired arterial inflow and chronic congestion.
2. Testicular Atrophy
While uncommon, testicular atrophy has been documented in rare post-vasectomy cases. Vascular compromise, especially when compounded by infection or hematoma, may lead to parenchymal loss over time. Histological studies from orchiectomy specimens of vasectomized individuals have occasionally revealed testicular fibrosis, decreased Leydig cell density, and seminiferous tubule degeneration — all of which are suggestive of ischemic injury.
3. Hormonal Fluctuations
Though vasectomy does not directly disrupt the hypothalamic-pituitary-gonadal axis, compromised testicular blood flow may secondarily impact hormone production. Leydig cells require a robust vascular supply for cholesterol transport and testosterone synthesis. Some studies have shown transient decreases in serum testosterone following vasectomy, though these are typically within physiological limits. Nonetheless, individuals with pre-existing vascular conditions or borderline testosterone levels may be more vulnerable to this subtle dysregulation.
Diagnostic Tools for Assessing Vascular Changes
1. Scrotal Doppler Ultrasound
This non-invasive imaging modality can assess testicular artery resistance, blood flow velocities, and venous drainage. Increased resistive index (RI > 0.7) is often considered a marker of compromised perfusion. Comparing pre- and post-vasectomy Doppler studies in longitudinal cohorts may offer valuable insight into vascular trajectory.
2. Contrast-Enhanced Ultrasound (CEUS)
CEUS provides high-resolution imaging of testicular microvascularity. It can detect subtle perfusion deficits not visible on conventional Doppler. Some pilot studies have identified delayed contrast wash-in and wash-out kinetics in vasectomized testes, suggesting microvascular remodeling.
3. MR Angiography
Though not routinely used, MR angiography offers superior visualization of deep spermatic cord vessels and surrounding fibrosis. It can be instrumental in complex PVPS cases or when surgical exploration is considered.
Therapeutic Considerations
If vascular dysregulation is suspected post-vasectomy, early intervention may mitigate long-term sequelae:
- NSAIDs and Corticosteroids: To suppress inflammatory responses and reduce vascular compression due to edema.
- Microsurgical Spermatic Cord Denervation (MSCD): For refractory pain linked to vascular or nerve entrapment.
- Reversal Surgery (Vasovasostomy): May decompress testicular structures and restore homeostasis in some patients, although evidence is mixed.
- Supportive Therapy: Scrotal elevation, anti-oxidants like CoQ10, and vasodilatory agents (in experimental settings) may have adjunctive roles.
Research Directions
While current data on vasectomy and testicular vascular dysregulation is limited, new research avenues are emerging:
- Longitudinal Imaging Studies: Following testicular blood flow patterns pre- and post-vasectomy could reveal subclinical trends.
- Biomarkers of Endothelial Dysfunction: Tracking levels of endothelin-1, NO, or VEGF may serve as indicators of vascular stress.
- Histopathological Correlation: Tissue-level changes post-vasectomy need systematic exploration in animal models and human biopsy samples.
The challenge lies in balancing the overwhelmingly positive risk-benefit profile of vasectomy as a contraceptive method with rare but significant vascular complications that can alter testicular physiology.
Conclusion
Vasectomy remains a cornerstone of male contraception, but its potential link to testicular vascular dysregulation deserves deeper clinical and scientific attention. Understanding the mechanisms of altered perfusion, inflammation-driven fibrosis, and venous congestion post-vasectomy can aid in better diagnosis, management, and possibly prevention of complications like PVPS or testicular atrophy.
Future work should focus on integrating imaging, molecular markers, and patient-reported outcomes to develop a comprehensive vascular health model in vasectomized men. For now, raising awareness among urologists and patients alike about testicular hemodynamics may lead to more personalized post-vasectomy care.
Frequently Asked Questions (FAQs)
1. Can vasectomy cause long-term damage to testicular blood vessels?
In most men, vasectomy does not lead to permanent vascular damage. However, in rare cases, inflammation or fibrosis around the vasectomy site may impact nearby vessels, leading to testicular vascular dysregulation. Monitoring symptoms like persistent pain or swelling is important.
2. How is testicular blood flow assessed after vasectomy?
Scrotal Doppler ultrasound is the most common method to assess testicular blood flow. It measures arterial resistance and velocity, helping detect vascular disturbances. In complex cases, contrast-enhanced ultrasound or MR angiography may be used.
3. What are the signs of vascular issues after vasectomy?
Common signs include chronic scrotal pain, a sensation of heaviness, swelling, or changes in testicular size. If these symptoms persist beyond three months post-procedure, a vascular evaluation may be warranted.

Leave a Reply